Francisco Church is a rehabilitation specialist and the chief editor of Recovery Ranger. He creates this site to offer guidance and support to individuals seeking...Read more
If you are struggling with addiction and are looking for help, you may be wondering how long you can stay in rehab with Medicare. The duration of your stay depends on a variety of factors, including the type of facility you choose, the severity of your addiction, and your overall health. In this article, we’ll discuss the factors that determine how long you can stay in rehab with Medicare, as well as other options that may be available to you. We’ll also discuss the importance of seeking professional help and the benefits of long-term recovery.
Contents
- Medicare Coverage for Stays in Rehab
- What Does Medicare Cover?
- What Is Not Covered by Medicare?
- What Are the Alternatives to Medicare Coverage?
- How to Obtain Medicare Coverage for a Stay in a Rehabilitation Facility
- Related Faq
- Q1: What is Medicare?
- Q2: How Long Can You Stay in Rehab With Medicare?
- Q3: Is There a Limit to How Many Days Medicare Will Cover in Rehab?
- Q4: What Types of Care Are Covered by Medicare in Rehab?
- Q5: Are There Any Exceptions to the 100-Day Limit for Medicare Rehab Coverage?
- Q6: What Is the Cost of Medicare Rehab Coverage?
- Medicare Benefits for Rehabilitation in a Skilled Nursing Facility
- Is Diethylpropion A Stimulant?
- Is Alcohol A Inflammatory?
- Does Alcohol Make A Uti Worse?
Medicare Coverage for Stays in Rehab
Rehabilitation facilities provide medical care, physical therapy, and psychological counseling to help patients recover from illnesses or injuries. For people with Medicare, the length of stay in a rehab facility is limited and depends on the type of setting. Medicare covers inpatient care in a skilled nursing facility, hospital, or rehabilitation facility; however, the coverage is limited and only covers medically necessary services.
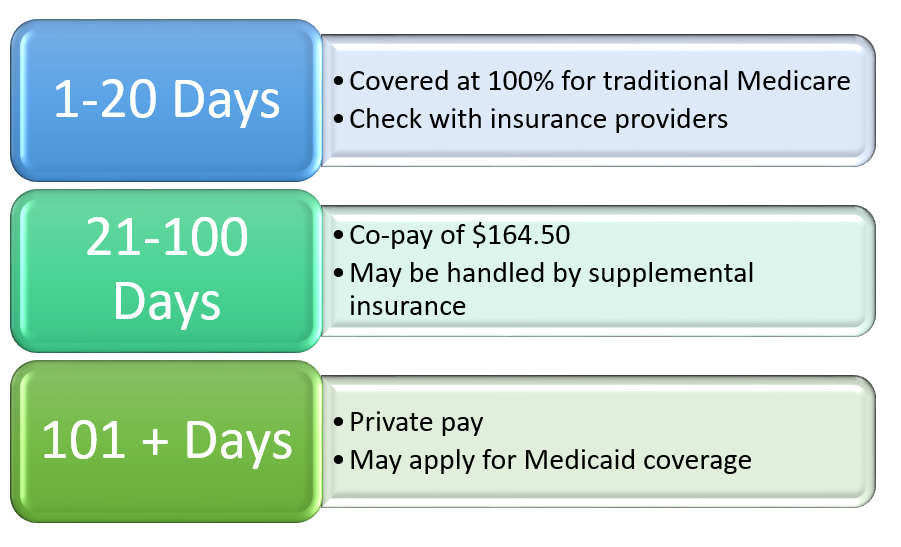
Medicare Part A covers up to 100 days of care in a skilled nursing facility or hospital. This coverage is provided for each benefit period and is subject to certain limits. For example, the first 20 days of a hospital stay are covered in full; however, beneficiaries will be responsible for a coinsurance payment for days 21 through 100. In a skilled nursing facility, coverage is provided for up to 100 days per benefit period, but there is a coinsurance payment for days 21 through 100.
In order to be eligible for Medicare coverage for a stay in a rehabilitation facility, the patient must have been admitted to a hospital for at least three days prior to the admission to the rehab facility. Medicare will cover the cost of up to 20 days of inpatient care in a rehabilitation facility, but there is a coinsurance payment for days 21 through 100.
What Does Medicare Cover?
Medicare covers inpatient care in a skilled nursing facility, hospital, or rehabilitation facility. This coverage is limited and only covers medically necessary services. Medicare Part A covers up to 100 days of care in a skilled nursing facility or hospital. This coverage is provided for each benefit period and is subject to certain limits. In order to be eligible for Medicare coverage for a stay in a rehabilitation facility, the patient must have been admitted to a hospital for at least three days prior to the admission to the rehab facility.
Medicare Part B covers certain medically necessary services, including physical and occupational therapy, speech-language pathology services, and outpatient services. Coverage for these services is limited, and beneficiaries may be subject to coinsurance payments and deductibles.
Medicare Part D covers prescription drugs. Coverage for prescription drugs is provided through private insurance companies that are approved by Medicare. Beneficiaries must pay a monthly premium for Part D coverage and may be subject to deductible and coinsurance payments.
What Is Not Covered by Medicare?
Medicare does not cover long-term care services or custodial care services. Long-term care services are those that are provided to individuals who require ongoing care due to a chronic illness or disability. Custodial care services are those that are provided to individuals who need help with activities of daily living, such as bathing, dressing, and eating.
Medicare does not cover the cost of private rooms, television, or telephone services in a hospital, skilled nursing facility, or rehabilitation facility. Medicare also does not cover the cost of transportation to and from medical appointments.
Medicare does not cover the cost of cosmetic surgery or experimental treatments. Medicare does not cover the cost of non-medically necessary services, such as massage therapy or acupuncture.
What Are the Alternatives to Medicare Coverage?
Those who are not eligible for Medicare may be able to obtain private insurance coverage for stays in a rehabilitation facility. Private insurance plans vary in terms of coverage and cost, so it is important to research the available plans before selecting one.
Many states offer Medicaid coverage for stays in a rehabilitation facility. Medicaid is a government-funded program that provides health care coverage to low-income individuals and families. Eligibility for Medicaid coverage varies from state to state, so it is important to check with the state Medicaid office to determine eligibility.
Some rehabilitation facilities may offer payment plans or discounts for those who are unable to pay for the stay in full. It is important to check with the facility to determine what payment options are available.
How to Obtain Medicare Coverage for a Stay in a Rehabilitation Facility
Step 1: Meet the Eligibility Requirements
In order to be eligible for Medicare coverage for a stay in a rehabilitation facility, the patient must have been admitted to a hospital for at least three days prior to the admission to the rehab facility. The patient must also be admitted to the rehab facility within 30 days of the hospital admission.
Step 2: Choose a Skilled Nursing Facility or Rehabilitation Facility
The patient or their family must choose a skilled nursing facility or rehabilitation facility that is approved by Medicare. It is important to research the facility to ensure that it meets the patient’s needs.
Step 3: Submit the Necessary Paperwork
The patient or their family must submit the necessary paperwork to the facility to apply for Medicare coverage. This paperwork includes the patient’s Medicare card, a completed application for Medicare coverage, the patient’s medical records, and any other documents that the facility may require.
Step 4: Contact Medicare
The patient or their family must contact Medicare to confirm that the patient is eligible for coverage. Medicare will provide information on the length of stay that is covered and any coinsurance payments that may be required.
Step 5: Make Payment Arrangements
Once eligibility for coverage has been confirmed, the patient or their family must make payment arrangements with the facility. Payment arrangements may include private insurance, Medicaid, a payment plan, or a discount.
Related Faq
Q1: What is Medicare?
A1: Medicare is a health insurance program administered by the federal government of the United States that covers certain medical expenses for citizens aged 65 and over, people under 65 with certain disabilities, and people with End-Stage Renal Disease (ESRD). Medicare is funded through payroll taxes and premiums paid by the insured.
Q2: How Long Can You Stay in Rehab With Medicare?
A2: The amount of time an individual can stay in rehab with Medicare depends on the type of care needed and the individual’s medical condition. Generally, Medicare covers up to 100 days of inpatient rehabilitation in an approved facility, but this is subject to certain conditions. Medicare will cover up to 20 days of inpatient rehab without the need for a deductible or coinsurance, but after that the patient is responsible for a coinsurance payment of up to $335 per day for the remaining 80 days.
Q3: Is There a Limit to How Many Days Medicare Will Cover in Rehab?
A3: Yes, Medicare has a limit to how many days they will cover in a rehabilitation facility. Generally, Medicare covers up to 100 days of inpatient rehabilitation in an approved facility, but this is subject to certain conditions. After the initial 20 days of inpatient rehab, the patient is responsible for a coinsurance payment of up to $335 per day for the remaining 80 days.
Q4: What Types of Care Are Covered by Medicare in Rehab?
A4: Medicare covers many types of care in a rehabilitation facility, including physical therapy, occupational therapy, speech-language therapy, and other medically-necessary services that are provided in an inpatient setting. Medicare also covers services such as medical social services, drugs, medical supplies, and durable medical equipment.
Q5: Are There Any Exceptions to the 100-Day Limit for Medicare Rehab Coverage?
A5: Yes, there are exceptions to the 100-day limit for Medicare rehab coverage. If a patient requires additional days of inpatient care beyond the 100-day limit, Medicare may cover those days if the care is medically necessary and the patient is deemed to have made “significant and measurable progress” while in rehab.
Q6: What Is the Cost of Medicare Rehab Coverage?
A6: The cost of Medicare rehab coverage depends on the type of care needed and the individual’s medical condition. Generally, Medicare covers up to 100 days of inpatient rehabilitation in an approved facility, but this is subject to certain conditions. Medicare will cover up to 20 days of inpatient rehab without the need for a deductible or coinsurance, but after that the patient is responsible for a coinsurance payment of up to $335 per day for the remaining 80 days.
Medicare Benefits for Rehabilitation in a Skilled Nursing Facility
When it comes to Medicare and rehab, the bottom line is that it is possible to stay for an extended period of time. However, it is important to note that the length of stay will depend on your individual needs and the facility you choose. It is also important to realize that Medicare will only cover a certain number of days, so it is important to do your research and understand your coverage. Armed with this knowledge, you can make an informed decision about how long you can stay in rehab with Medicare.
Francisco Church is a rehabilitation specialist and the chief editor of Recovery Ranger. He creates this site to offer guidance and support to individuals seeking to overcome addiction and achieve lasting sobriety. With extensive experience in the field of addiction treatment, Francisco is dedicated to helping individuals access the resources they need for successful recovery.
- Latest Posts by Francisco Church
-
Is Diethylpropion A Stimulant?
- -
Is Alcohol A Inflammatory?
- -
Does Alcohol Make A Uti Worse?
- All Posts