Francisco Church is a rehabilitation specialist and the chief editor of Recovery Ranger. He creates this site to offer guidance and support to individuals seeking...Read more
Mental health is a critical component of overall wellbeing, and many people require counseling in order to achieve the best results. Unfortunately, mental health counseling can be expensive, which can leave individuals feeling helpless and overwhelmed. Fortunately, Medicare does offer coverage for mental health counseling services, so for those who qualify, the financial burden of mental health care can be significantly reduced. In this article, we will explore the specifics of what Medicare covers for mental health counseling.
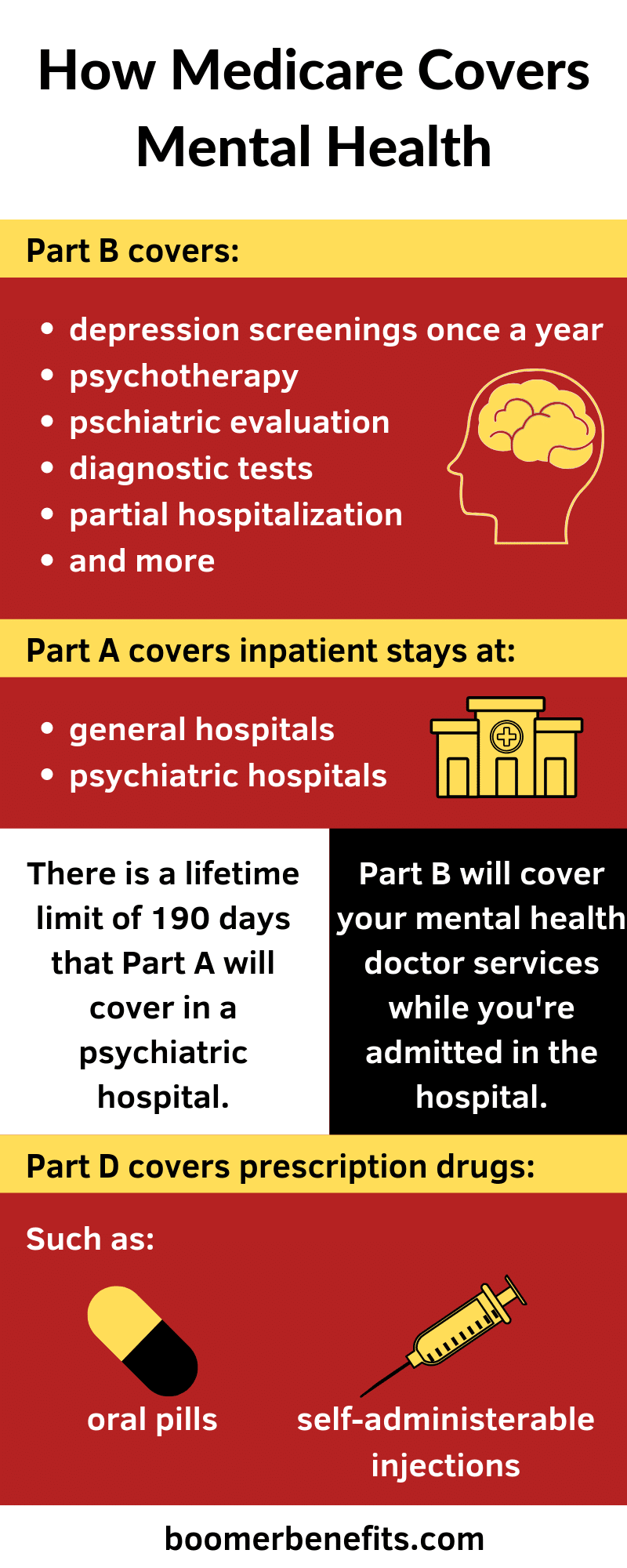
Yes, Medicare covers mental health counseling. Medicare Part B (Medical Insurance) helps pay for outpatient mental health services, including services that help you diagnose and treat mental health conditions. You pay a coinsurance or copayment for these services. Medicare covers these services when they’re medically necessary.
Contents
- Does Medicare Cover Mental Health Counseling?
- Related Faq
- Does Medicare Cover Mental Health Counseling?
- What Mental Health Counseling Does Medicare Cover?
- What is the Cost of Mental Health Counseling with Medicare?
- Are All Mental Health Counseling Services Covered by Medicare?
- Do I Need a Referral for Mental Health Counseling with Medicare?
- What Documents Do I Need to Submit for Mental Health Counseling with Medicare?
- Medicare Behavioral Health Coverage
- Is Diethylpropion A Stimulant?
- Is Alcohol A Inflammatory?
- Does Alcohol Make A Uti Worse?
Does Medicare Cover Mental Health Counseling?
Mental health counseling is an essential part of any person’s well-being, but many people are unaware of the coverage that Medicare provides for mental health counseling. Medicare covers some mental health services such as counseling, psychiatry, and psychotherapy, but the coverage varies depending on the type of mental health services received and the type of Medicare plan. In this article, we will discuss what types of mental health services Medicare covers, how to determine if a service is covered, and how to get the most out of Medicare coverage for mental health counseling.
Types of Mental Health Services Covered by Medicare
Medicare covers a variety of mental health services, including counseling, psychiatry, and psychotherapy. Counseling is typically provided in individual or group sessions by a mental health professional. Psychiatry is a type of care provided by a physician who specializes in mental health and can provide medication as well as therapy. Psychotherapy is a type of mental health counseling that focuses on treating mental health issues through talk therapy.
How to Determine if a Mental Health Service is Covered
In order to determine if a mental health service is covered by Medicare, you should first contact your Medicare plan provider or the Medicare hotline to find out what services are covered and what the eligibility requirements are for each service. You should also ask your provider about any additional costs associated with the service, such as co-pays and deductibles. Additionally, you should ask your provider if there are any restrictions on the number of sessions covered or if there are any limits on the types of services covered.
How to Get the Most Out of Medicare Coverage for Mental Health Counseling
In order to get the most out of your Medicare coverage for mental health counseling, it is important to understand the types of services that are covered and the eligibility requirements associated with each service. You should also make sure to keep track of all costs associated with the service, such as co-pays and deductibles, and ask your provider about any limits on the number of sessions. Additionally, it is important to be aware of any restrictions on the types of services covered by your plan and to discuss any questions or concerns you have with your provider.
Finding a Mental Health Provider That Accepts Medicare
If you are looking for a mental health provider that accepts Medicare, you should contact your Medicare plan provider or the Medicare hotline to find out which providers in your area accept Medicare. Additionally, you can search for providers online or contact your local mental health association for a list of providers. Once you have found a provider that accepts Medicare, you should contact them to discuss the services they offer and any additional costs associated with the service.
Conclusion
Medicare provides coverage for a variety of mental health services, including counseling, psychiatry, and psychotherapy. It is important to understand what services are covered by Medicare and the eligibility requirements associated with each service. Additionally, you should keep track of all costs associated with the service, such as co-pays and deductibles, and ask your provider about any limits on the number of sessions. Finally, it is important to find a mental health provider that accepts Medicare and to discuss any questions or concerns you have with your provider.
Related Faq
Does Medicare Cover Mental Health Counseling?
Answer: Yes, Medicare does cover mental health counseling. Medicare Part B covers 80% of the cost of outpatient mental health services, such as individual and group therapy. Some Medicare Advantage plans may also cover mental health counseling.
What Mental Health Counseling Does Medicare Cover?
Answer: Medicare Part B covers 80% of the cost of outpatient mental health services, such as individual and group therapy, provided by psychologists, clinical social workers, or licensed clinical counselors. Medicare does not cover services provided by psychiatrists. Medicare Advantage plans may cover additional types of mental health counseling services.
What is the Cost of Mental Health Counseling with Medicare?
Answer: Medicare Part B pays 80% of the Medicare-approved amount for outpatient mental health services, and you are responsible for the remaining 20%. The cost of mental health counseling can vary based on the provider, location, and type of service. Some Medicare Advantage plans may cover additional costs associated with mental health counseling.
Are All Mental Health Counseling Services Covered by Medicare?
Answer: No, not all mental health counseling services are covered by Medicare. Medicare does not cover services provided by psychiatrists, and some Medicare Advantage plans may only cover certain types of mental health counseling services. It is important to check with your provider to see what services are covered by Medicare.
Do I Need a Referral for Mental Health Counseling with Medicare?
Answer: No, you do not need a referral for mental health counseling with Medicare. Medicare Part B covers 80% of the cost of outpatient mental health services, such as individual and group therapy, provided by psychologists, clinical social workers, or licensed clinical counselors. Some Medicare Advantage plans may require a referral for mental health counseling.
What Documents Do I Need to Submit for Mental Health Counseling with Medicare?
Answer: For mental health counseling services covered by Medicare Part B, you will need to submit a claim form, an itemized bill, and any other required documents. You will also need to provide proof of your Medicare coverage and a copy of your Medicare card. Medicare Advantage plans may require additional documentation to be submitted with your claim.
Medicare Behavioral Health Coverage
After exploring the question of whether Medicare covers mental health counseling, it is clear that the answer is yes. It is important to note, however, that the extent to which Medicare covers mental health counseling depends on the individual policy and the type of counseling sought. To ensure that mental health counseling is adequately covered, it is important to speak with a Medicare representative and read the policy carefully. With the right coverage in place, Medicare can provide the necessary resources to help individuals receive the mental health counseling they need.
Francisco Church is a rehabilitation specialist and the chief editor of Recovery Ranger. He creates this site to offer guidance and support to individuals seeking to overcome addiction and achieve lasting sobriety. With extensive experience in the field of addiction treatment, Francisco is dedicated to helping individuals access the resources they need for successful recovery.
- Latest Posts by Francisco Church
-
Is Diethylpropion A Stimulant?
- -
Is Alcohol A Inflammatory?
- -
Does Alcohol Make A Uti Worse?
- All Posts