Francisco Church is a rehabilitation specialist and the chief editor of Recovery Ranger. He creates this site to offer guidance and support to individuals seeking...Read more
Mental health is an important and often overlooked aspect of health. Unfortunately, many people cannot afford the cost of mental health treatments. Thankfully, Medicaid is an insurance program that may provide financial assistance to those in need. This article will explore whether Medicaid covers inpatient mental health services. We will look at the benefits, costs, and eligibility criteria for Medicaid’s inpatient mental health services. By the end of the article, you will have a better understanding of whether Medicaid is an option for you or a loved one when it comes to seeking inpatient mental health care.
Medicaid covers inpatient mental health care if the services are deemed medically necessary and are provided in an approved hospital or other inpatient facility. The services must be provided in accordance with the Medicaid state plan, which sets out the specific services and requirements for eligibility. Medicaid may also cover services such as diagnosis and treatment of mental health conditions, psychotherapy, and other medically necessary services. To find out if you are eligible for Medicaid coverage of inpatient mental health care, contact your state Medicaid office.
Contents
- Does Medicaid Cover Inpatient Mental Health Treatment?
- Related Faq
- Does Medicaid Cover Inpatient Mental Health?
- What type of mental health care does Medicaid cover?
- What types of facilities does Medicaid cover for inpatient mental health care?
- How do I know if I am eligible for Medicaid coverage for inpatient mental health care?
- What if I need inpatient mental health care but I am not eligible for Medicaid?
- What types of mental health care providers does Medicaid cover?
- Medicare Behavioral Health Coverage
- Is Diethylpropion A Stimulant?
- Is Alcohol A Inflammatory?
- Does Alcohol Make A Uti Worse?
Does Medicaid Cover Inpatient Mental Health Treatment?
Inpatient mental health treatment includes a range of services that provide care in a secure facility for people with severe mental health issues. These services can include medication management, therapy, and other forms of support. In some cases, inpatient mental health treatment may be necessary in order to get someone on the road to recovery. Fortunately, Medicaid, the federal health insurance program for lower-income individuals and families, does cover inpatient mental health treatment.
Medicaid coverage for inpatient mental health treatment varies from state to state. Generally, Medicaid will cover the cost of inpatient hospital stays for mental health treatment, as well as medication, individual and group therapy, and any other services necessary to treat the individual’s mental health condition. However, Medicaid may not cover all of the costs associated with inpatient mental health treatment. In some cases, it may require the patient to pay a copayment for their care.
What Types of Mental Health Treatment Does Medicaid Cover?
Medicaid typically covers a wide range of inpatient mental health treatment services, including individual and group therapy, medication management, and any other service that is necessary to treat the individual’s mental health condition. Medicaid may also cover the cost of any medical tests or lab work that is necessary to diagnose and treat a mental health condition.
In addition, Medicaid may also cover the cost of any medical equipment or supplies that are necessary for inpatient mental health treatment. This may include items such as wheelchairs, walkers, hearing aids, and other types of medical devices. Medicaid may also cover the cost of any necessary transportation to and from the inpatient mental health facility.
Are There Any Limitations on Medicaid Coverage for Inpatient Mental Health Treatment?
In most cases, Medicaid will cover the cost of inpatient mental health treatment, but there may be some limitations. For example, some states may only cover inpatient mental health treatment for a certain amount of time. Other states may require a copayment for inpatient mental health treatment. Additionally, there may be limits on the types of services that Medicaid will cover for inpatient mental health treatment. It is important to check with your state Medicaid program to determine what services are covered and any limitations that may apply.
What Documents Do I Need to Obtain Medicaid Coverage for Inpatient Mental Health Treatment?
In order to obtain Medicaid coverage for inpatient mental health treatment, you will need to provide the following documents to your state Medicaid program:
Proof of Medicaid Eligibility
You will need to provide proof of your eligibility for Medicaid in order to obtain coverage for inpatient mental health treatment. This may include proof of your income, proof of citizenship or legal residency, and any other documents that are required by your state Medicaid program.
Medical Documentation
You will also need to provide documentation from your doctor that states that inpatient mental health treatment is necessary. This documentation should include a detailed description of your mental health condition and any other information that is necessary for Medicaid to approve your coverage for inpatient mental health treatment.
Mental Health Treatment Plan
You will also need to provide a detailed mental health treatment plan that outlines the type of treatment that you will receive and the length of time that you will be receiving treatment. This plan should include a description of any medications that will be prescribed, any individual or group therapy sessions that you will be attending, and any other services that will be provided as part of your treatment.
Related Faq
Does Medicaid Cover Inpatient Mental Health?
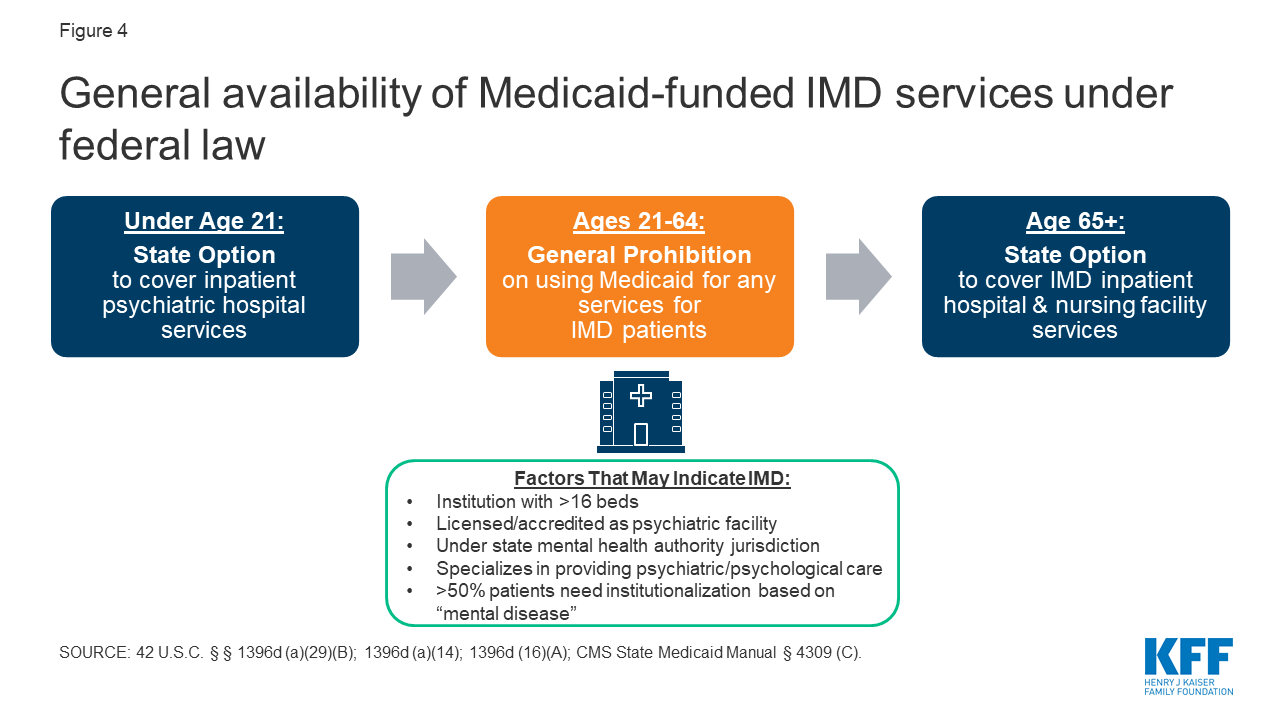
Answer: Yes, Medicaid does cover inpatient mental health care. Depending on the state, Medicaid may cover inpatient mental health care in a variety of settings, including inpatient psychiatric hospitals, residential treatment centers, and nursing homes. Medicaid also covers a variety of mental health services, including inpatient and outpatient counseling, psychotherapy, case management, and medication management.
What type of mental health care does Medicaid cover?
Answer: Medicaid covers a variety of mental health care services, including inpatient and outpatient counseling, psychotherapy, case management, and medication management. In addition, depending on the state, Medicaid may cover inpatient mental health care in a variety of settings, including inpatient psychiatric hospitals, residential treatment centers, and nursing homes.
What types of facilities does Medicaid cover for inpatient mental health care?
Answer: Depending on the state, Medicaid may cover inpatient mental health care in a variety of settings, including inpatient psychiatric hospitals, residential treatment centers, and nursing homes. Inpatient psychiatric hospitals provide 24-hour care from psychiatrists and other mental health professionals, while residential treatment centers provide a more structured environment with daily support from mental health professionals. Nursing homes provide a less intensive form of care, with around-the-clock supervision from medical personnel.
How do I know if I am eligible for Medicaid coverage for inpatient mental health care?
Answer: Eligibility for Medicaid coverage for inpatient mental health care varies by state. Generally, you must meet certain income and resource requirements and be diagnosed with a mental health condition to be eligible for Medicaid coverage. To find out if you are eligible for Medicaid coverage for inpatient mental health care in your state, contact your state’s Medicaid office.
What if I need inpatient mental health care but I am not eligible for Medicaid?
Answer: If you need inpatient mental health care but you are not eligible for Medicaid, you may be able to find assistance through other sources. Some states offer mental health services through their state health departments or mental health authorities. If you have private health insurance, you may also be able to find coverage for inpatient mental health care through your insurance provider. Additionally, many mental health care providers offer sliding scale payments for those who are unable to pay for services.
What types of mental health care providers does Medicaid cover?
Answer: Medicaid generally covers a variety of mental health care providers, including psychiatrists, psychologists, social workers, counselors, and other mental health professionals. In addition, Medicaid may cover services provided by facilities that specialize in mental health care, such as inpatient psychiatric hospitals and residential treatment centers. Your state’s Medicaid office can provide more information about the types of mental health care providers that are covered by Medicaid in your area.
Medicare Behavioral Health Coverage
In conclusion, Medicaid does cover inpatient mental health in some cases, depending on the state and the individual’s circumstances. While Medicaid coverage for inpatient mental health varies state-by-state, it is important to make sure to check with your state’s Medicaid office to fully understand the coverage provided and any eligibility requirements. By doing so, you can ensure you get the care you need for any inpatient mental health services.
Francisco Church is a rehabilitation specialist and the chief editor of Recovery Ranger. He creates this site to offer guidance and support to individuals seeking to overcome addiction and achieve lasting sobriety. With extensive experience in the field of addiction treatment, Francisco is dedicated to helping individuals access the resources they need for successful recovery.
- Latest Posts by Francisco Church
-
Is Diethylpropion A Stimulant?
- -
Is Alcohol A Inflammatory?
- -
Does Alcohol Make A Uti Worse?
- All Posts