Francisco Church is a rehabilitation specialist and the chief editor of Recovery Ranger. He creates this site to offer guidance and support to individuals seeking...Read more
Mental health is an important aspect of our lives, and it is essential to ensure that we have access to the care and resources we need to stay healthy and balanced. With advances in healthcare and the increasing availability of mental health services, many people are wondering if their health insurance plan covers mental health therapy. In this article, we will explore the question of whether Anthem health insurance covers mental health therapy. We will discuss the various types of mental health services that may be covered as well as any potential restrictions or exclusions that may apply.
Yes, Anthem covers mental health therapy. Anthem’s mental health coverage includes services such as individual and group therapy, family counseling, and inpatient and outpatient care. Anthem also offers programs and resources to help you manage mental health issues and find the right treatment. Anthem’s mental health coverage is subject to your specific plan’s benefits, so be sure to check with your plan to determine coverage and costs.
Contents
- Does Anthem Cover Mental Health Therapy?
- Few Frequently Asked Questions
- Does Anthem Cover Mental Health Therapy?
- What Types Of Mental Health Services Are Covered By Anthem?
- Do I Need A Referral For Mental Health Services Through Anthem?
- What Is The Cost Of Mental Health Services Through Anthem?
- What Is The Process For Filing A Mental Health Claim Through Anthem?
- Can I Use My Anthem Mental Health Benefits Out-Of-Network?
- Is Diethylpropion A Stimulant?
- Is Alcohol A Inflammatory?
- Does Alcohol Make A Uti Worse?
Does Anthem Cover Mental Health Therapy?
Mental health is an important part of overall health and well-being. Anthem, one of the largest health insurance providers in the US, offers coverage for mental health services. This article will discuss what mental health therapy is, what types of mental health services are covered under Anthem, and how to access mental health services through Anthem.
What is Mental Health Therapy?
Mental health therapy, also known as psychotherapy, is a type of treatment that uses talk therapy to help people better understand and cope with emotional or psychological problems. Mental health therapy can help people manage and reduce symptoms of mental health disorders, such as depression, anxiety, and post-traumatic stress disorder (PTSD). It can also help individuals develop healthy coping skills and learn to better manage stress.
What Types of Mental Health Services Does Anthem Cover?
Anthem covers a variety of mental health services. These services include individual counseling, family counseling, couples counseling, and group therapy. Anthem also covers diagnostic assessments, medication management, and crisis intervention.
Anthem also covers alternative types of mental health therapy, such as art therapy, music therapy, and animal-assisted therapy. These alternative therapies can be beneficial for individuals who may not respond to traditional talk therapy.
How to Access Mental Health Services Through Anthem
If you are an Anthem member and are seeking mental health services, you should first contact your primary care physician. Your doctor can help you determine if you are eligible for mental health services under your Anthem plan.
If you are eligible, your doctor can refer you to an in-network mental health provider who is covered by your Anthem plan. You can also search for an in-network mental health provider on Anthem’s website.
What Costs Are Associated With Mental Health Services?
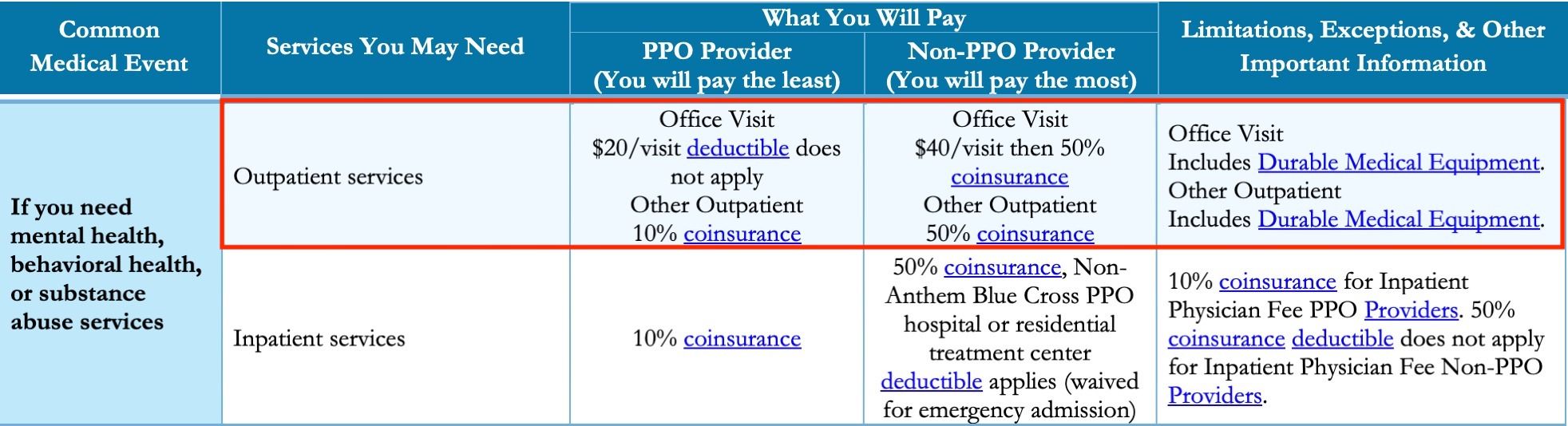
The cost of mental health services can vary depending on your Anthem plan. Generally, you will be responsible for a copayment or coinsurance for each mental health service you receive. You may also be responsible for a deductible if you have not yet met your plan’s annual deductible.
Are Mental Health Services Covered Out-of-Network?
Anthem may cover some mental health services when they are provided by an out-of-network provider. However, the cost of out-of-network services may be higher than those provided by an in-network provider. Additionally, out-of-network providers may not accept Anthem’s negotiated rates, which could result in higher out-of-pocket costs for you.
What if I Need Additional Mental Health Services?
If you need additional mental health services, such as long-term therapy or residential treatment, you may be able to get coverage through Anthem’s Behavioral Health Services program. This program offers expanded coverage for mental health services, including residential treatment and long-term therapy. To learn more about the Behavioral Health Services program, you can contact Anthem’s customer service team.
Conclusion
Anthem offers coverage for a variety of mental health services, including individual counseling, family counseling, alternative therapies, and more. To access these services, you should contact your primary care physician and ask if you are eligible for mental health services through your Anthem plan. If you need additional mental health services, such as long-term therapy or residential treatment, you may be able to get coverage through Anthem’s Behavioral Health Services program.
Few Frequently Asked Questions
Does Anthem Cover Mental Health Therapy?
Yes, Anthem does cover mental health therapy. Anthem offers a broad range of mental health services for both in-network and out-of-network providers. Depending on the plan, Anthem covers services such as individual therapy, couples therapy, family therapy, and group therapy. In addition, Anthem also covers psychiatric evaluations and medication management.
What Types Of Mental Health Services Are Covered By Anthem?
Anthem covers a broad range of mental health services, including individual therapy, couples therapy, family therapy, group therapy, psychiatric evaluations, and medication management. Anthem also covers some holistic therapies such as art therapy, music therapy, and yoga therapy. Anthem also covers telehealth services such as counseling, psychiatry, and psychotherapy.
Do I Need A Referral For Mental Health Services Through Anthem?
No, you do not need a referral for mental health services through Anthem. However, depending on the specific plan, a referral may be required for certain services or a referral may be required for services from an out-of-network provider.
What Is The Cost Of Mental Health Services Through Anthem?
The cost of mental health services through Anthem will vary depending on the specific plan and the type of service. Typically, Anthem covers a portion of the cost, and the remaining cost is the responsibility of the patient. Anthem also offers discounts for some services, such as telehealth services.
What Is The Process For Filing A Mental Health Claim Through Anthem?
The process for filing a mental health claim through Anthem is relatively straightforward. First, the patient must receive the service and pay the provider. The patient then submits a claim to Anthem with proof of payment, such as a receipt or invoice. Anthem will then review the claim and reimburse the patient for the portion of the cost that is covered by the plan.
Can I Use My Anthem Mental Health Benefits Out-Of-Network?
Yes, you can use your Anthem mental health benefits out-of-network. However, out-of-network services typically cost more and may require a referral from a primary care physician. Additionally, Anthem will typically only cover a portion of the cost of out-of-network services, and the remaining cost is the responsibility of the patient.
In conclusion, we can see that Anthem does indeed cover mental health therapy, provided it is deemed medically necessary for the individual. This coverage is often determined by the individual’s doctor, who will assess the situation to decide if mental health therapy is appropriate. Anthem also has a range of mental health benefits, such as free access to a mental health helpline, in-network mental health professionals and coverage for both inpatient and outpatient mental health services. All in all, Anthem is a great choice for those who are in need of mental health therapy coverage.
Francisco Church is a rehabilitation specialist and the chief editor of Recovery Ranger. He creates this site to offer guidance and support to individuals seeking to overcome addiction and achieve lasting sobriety. With extensive experience in the field of addiction treatment, Francisco is dedicated to helping individuals access the resources they need for successful recovery.
- Latest Posts by Francisco Church
-
Is Diethylpropion A Stimulant?
- -
Is Alcohol A Inflammatory?
- -
Does Alcohol Make A Uti Worse?
- All Posts