Francisco Church is a rehabilitation specialist and the chief editor of Recovery Ranger. He creates this site to offer guidance and support to individuals seeking...Read more
As mental health issues become increasingly pervasive in our society, it is important to know what kind of coverage your insurance provides. One of the most popular health insurance companies is Aetna, so it is natural to wonder: Does Aetna cover mental health? Fortunately, Aetna has one of the most comprehensive mental health coverage options out there, providing coverage for a wide range of mental health services. Let’s take a closer look at what Aetna covers and the benefits of their mental health coverage.
Yes, Aetna covers mental health services. Aetna offers a wide range of mental health services, including medication management, therapy, and group counseling. Aetna also covers treatment for substance abuse and addiction. To find out what services and treatments are covered in your plan, contact Aetna Member Services.
Contents
- Does Aetna Offer Mental Health Insurance Benefits?
- Does Aetna Offer Mental Health Insurance Plans?
- Related Faq
- Does Aetna Cover Mental Health?
- What Types of Mental Health Services Does Aetna Cover?
- How Much Does Aetna Cover for Mental Health Services?
- What Are the Exclusions for Mental Health Coverage with Aetna?
- Are Telehealth Services Covered by Aetna Mental Health Coverage?
- What Is Required to Access Mental Health Services Through Aetna?
- Is Diethylpropion A Stimulant?
- Is Alcohol A Inflammatory?
- Does Alcohol Make A Uti Worse?
Does Aetna Offer Mental Health Insurance Benefits?
Aetna is a health insurance provider that offers a variety of policies, including those for mental health services. Mental health coverage is an important part of any insurance policy, and Aetna’s plans provide coverage for a variety of mental health services, including therapy, medication, and hospitalization. Knowing what kind of coverage you can expect from Aetna can help you decide which policy is right for you.
What Mental Health Services Does Aetna Cover?
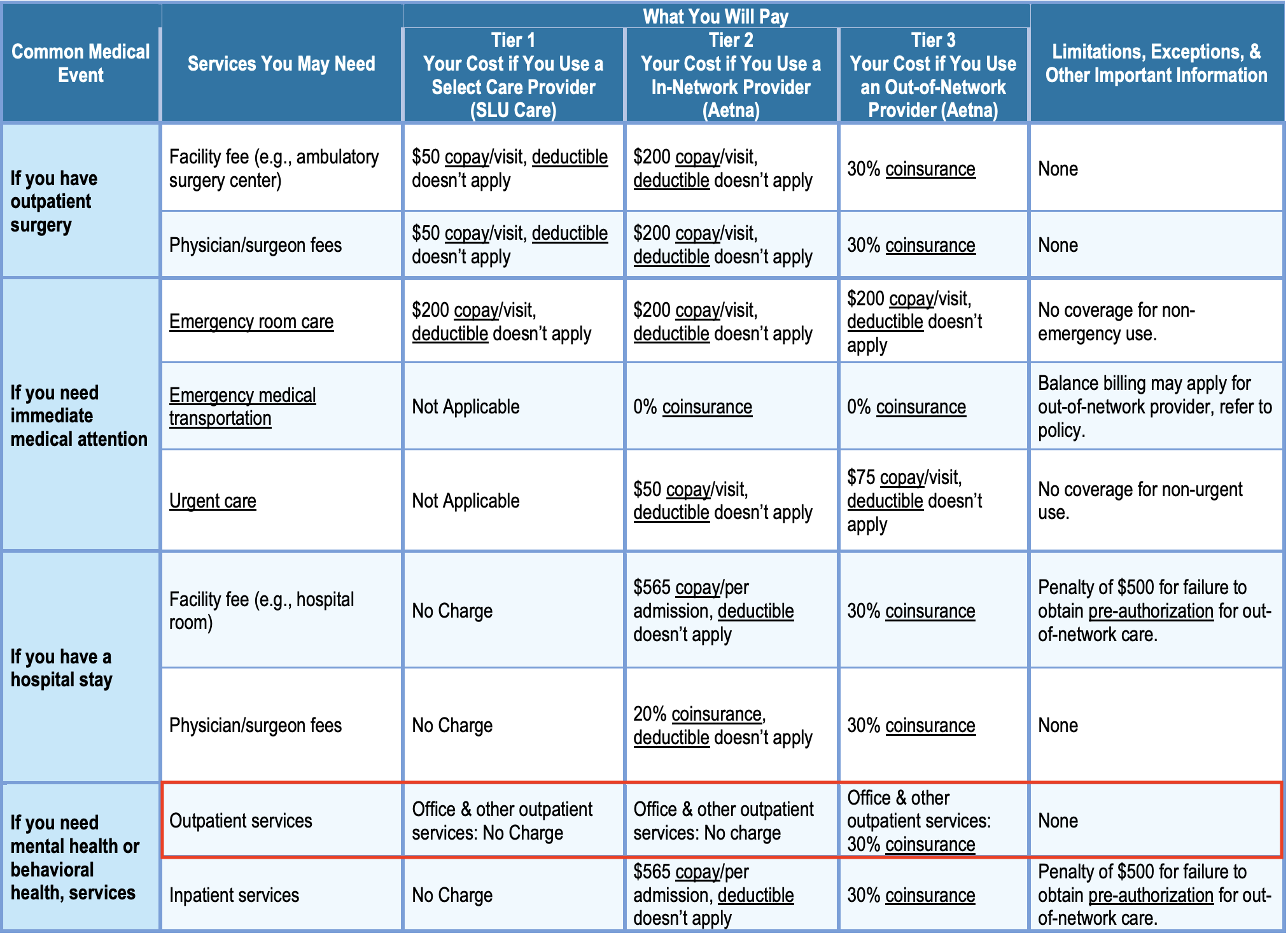
Aetna offers coverage for a wide range of mental health services. This includes inpatient and outpatient services, such as therapy sessions, psychologist visits, and medication. Aetna also offers coverage for hospitalization related to mental health, including emergency situations. Additionally, Aetna covers mental health screenings and assessments, as well as services related to substance abuse or addiction.
Are There Any Limitations on Mental Health Coverage?
In some cases, Aetna does place limits on mental health coverage. For example, there may be limits on the number of visits to a therapist or the number of days of hospitalization covered. Additionally, some services may not be covered at all, such as alternative treatments like acupuncture or yoga. It’s important to check your policy to make sure you understand what is and isn’t covered.
Does Aetna Offer Mental Health Insurance Plans?
Aetna offers a variety of plans that include coverage for mental health services. These plans vary in terms of deductible amounts and copays, as well as the amount of coverage for mental health services. Additionally, some plans may include coverage for preventive services, such as mental health screenings and assessments. Checking with Aetna’s customer service team can help you determine which plan is best for you.
Are There Any Additional Benefits for Mental Health Services?
Aetna also offers additional benefits for mental health services, such as discounted rates for certain services and access to online mental health programs. Additionally, some Aetna plans may provide coverage for alternative treatments, such as acupuncture or yoga. It’s important to check your policy to make sure you understand what is and isn’t covered.
Do I Need a Referral for Mental Health Services?
In some cases, you may need a referral from a primary care physician in order to receive coverage for mental health services. If this is the case, your primary care physician will need to provide a referral to a mental health provider in order for you to receive coverage. It’s important to check with your insurance company to make sure you understand the requirements for mental health coverage.
Related Faq
Does Aetna Cover Mental Health?
Answer: Yes, Aetna does cover mental health. Aetna offers a wide range of mental health coverage options including inpatient and outpatient care, prescription drugs, in-network providers, and more. Aetna covers up to 90% of the cost of mental health services when you use in-network providers. Out-of-network providers may be covered, but you will pay a higher percentage of the cost.
What Types of Mental Health Services Does Aetna Cover?
Answer: Aetna covers a wide range of mental health services, including inpatient and outpatient care, prescription drugs, in-network providers, and more. Inpatient services may include hospitalization, residential treatment, and partial hospitalization. Outpatient services may include individual, family, or group therapy and counseling, as well as occupational therapy, psychological testing, and psychiatric evaluation. Aetna also covers prescription drugs for mental health issues.
How Much Does Aetna Cover for Mental Health Services?
Answer: Aetna covers up to 90% of the cost of mental health services when you use in-network providers. Out-of-network providers may be covered, but you will pay a higher percentage of the cost. However, the amount of coverage you receive depends on your plan and your current health status. It is best to review your policy and contact Aetna to find out what your coverage is and what the cost will be.
What Are the Exclusions for Mental Health Coverage with Aetna?
Answer: Aetna does not cover services or treatments that are not medically necessary, experimental, or not specifically listed in your plan. Aetna also does not cover services related to substance abuse or treatments that are not considered to be evidence-based. Additionally, some mental health services may be affected by limits or caps on the amount of coverage you can receive.
Are Telehealth Services Covered by Aetna Mental Health Coverage?
Answer: Yes, Aetna does cover telehealth services for mental health issues. Telehealth services allow you to access mental health services from the comfort of your own home. These services may include individual, family, or group therapy, as well as occupational therapy, psychological testing, and psychiatric evaluation. However, the coverage of these services may vary depending on your plan and your current health status.
What Is Required to Access Mental Health Services Through Aetna?
Answer: To access mental health services through Aetna, you must first be enrolled in an Aetna health plan. You will then need to contact Aetna to find a mental health care provider in your network. Once you have found a provider, you will need to schedule an appointment and provide your Aetna health plan information at the time of your appointment. You may also need to provide additional documentation related to your mental health condition before your coverage can be activated.
In conclusion, Aetna does cover mental health services, depending on the specific plan you have. They offer a variety of different coverage options to meet the needs of their customers, from basic to comprehensive coverage. Aetna is committed to providing quality health care and services to their members, and mental health is no exception. If you are considering Aetna coverage, be sure to review your plan to make sure it meets your mental health needs.
Francisco Church is a rehabilitation specialist and the chief editor of Recovery Ranger. He creates this site to offer guidance and support to individuals seeking to overcome addiction and achieve lasting sobriety. With extensive experience in the field of addiction treatment, Francisco is dedicated to helping individuals access the resources they need for successful recovery.
- Latest Posts by Francisco Church
-
Is Diethylpropion A Stimulant?
- -
Is Alcohol A Inflammatory?
- -
Does Alcohol Make A Uti Worse?
- All Posts